Astrocytoma causes are currently unknown. There are some supposed risk factors, such as genetic factors. For instance, children with neurofibromatosis are thought to have a higher risk of developing an astrocytoma.
Imaging tests which may be used include: 1. Computed tomography scan (CT or CAT), 2. Magnetic resonance imaging (MRI)
Once a tumor is detected, a biopsy is taken, which may occur by itself, or in some cases during the surgery to remove the tumor. Staging of the tumor is done through examination of the sample removed during biopsy.
Astrocytoma treatment varies depending upon the particular case, in individual, whether the tumor is benign or malignant (cancer), etc. Surgery is the most common treatment method, although radiation treatment, chemotherapy, and other options do exist.
Different grading systems are used for classification of astrocytomas.
An ependymoma is a tumor that arises from cells of the ependymal lining of the ventricular system of brain or spinal cord. The ventricular system contains cerebrospinal fluid (CSF).
The average age at diagnosis is 5 years old, and 25-40 percent of patients are less than 2 years old. Ependymomas occur equally in males and females.
Ependymomas account for 5-10 percent of pediatric brain tumors. Approximately 60 percent are located in the region of the cerebellum and brain stem known as the posterior fossa, 10 percent are located in the spinal cord, and the remaining 30 percent in other parts of the brain. Ependymomas account for 25 percent of all spinal cord tumors. Most patients with tumors of the spinal cord are older than 12 years.
As you read further below, you will find general information about ependymomas. If you would like to view summary information about brain tumors first, see the overview on brain tumors.
Symptoms vary depending on size and location of tumor. Tumor can block the normal flow of CSF, causing increased pressure on the brain (hydrocephalus) and enlargement of the skull and a variety of symptoms. Common symptoms may include:
The symptoms of a brain tumor may resemble other conditions or medical problems - ranging from the simple to the serious. Always consult your child's physician for diagnosis and treatment.
Microscopically, ependymomas can appear different, called either standard or anaplastic ependymoma. These two types are treated the same and have approximately the same prognosis.
A third type, which occurs at the base of the spine, called myxopapillary cauda equina ependymoma, tends to be much less malignant than any of the other forms. A fourth type, called ependymoblastoma, is a more aggressive form of this tumor and more difficult to treat. Its diagnosis and management are similar to that of primitive neuroectodermal tumor (PNET) and is discussed in the section on PNET.
Ependymomas can metastasize, meaning they can spread into adjacent areas of the brain or, less commonly, to distant parts of the central nervous system. Approximately 12 percent of patients will have evidence of spread of disease at diagnosis. In these situations, more extensive treatment is used to cure the disease.
Diagnostic procedures for an ependymoma, like other brain tumors, are necessary to determine the exact type of tumor and whether the tumor has spread. These may include:
Scans - magnetic resonance imaging (MRI) scans are obtained using computerized, large magnetic fields to produce detailed images of organs and structures within the body. This will provide information on the location, size and characteristics of the tumor. The magnetic fields are not harmful and are safer than even routine x-rays. Computerized tomography (CT) or CAT scans using x-rays are also occasionally used.
Biopsy - a tissue sample from the tumor taken during surgery to remove part or all of the tumor. The sample will provide definitive information about the type of tumor.
lumbar puncture (spinal tap) - to remove a small sample of cerebrospinal fluid (CSF), a special needle is placed into the lower back, into the spinal canal, the area around the spinal cord. CSF is the fluid that bathes the brain and spinal cord. The sample is sent for testing to determine if any tumor cells have started to spread. In children, this procedure is safely performed under sedation, and is less difficult and less painful than placing an intravenous (IV) catheter.
Specific treatment to cure ependymoma will be determined by your child's physician based on:
- Type, location, and size of the tumor
- Extent of the disease
- Your child's age, overall health, and medical history
- How your child's doctors expect the disease to progress
- Your child's tolerance for specific medications, procedures, or therapies
- Your preference and judgement
Treatment approaches include:
Surgery - usually the first step and mainstay in the treatment of brain tumors. The goal is to remove as much of the tumor as possible while preserving neurological function. Tumor specimens are examined by neuropathologists to determine the exact diagnosis. Complete resection or surgical removal of the entire tumor is ideal when this is feasible. However, tumor location and other characteristics may limit removal to a partial or sub-total resection. A biopsy is the surgical removal of a sample of the tumor for diagnostic purposes. This is frequently done if the tumor is in an area with sensitive structures around it that may be injured during removal. In general, the more complete the resection, the better the chances for cure.
Ventriculo-peritoneal shunt (VP shunt) - when a tumor causes blockage of CSF flow leading to symptoms, special tubing can be surgically implanted in the ventricles to drain excess CSF into the abdomen. This bypasses the tumor blockage and relieves symptoms of hydrocephalus.
Radiation therapy - precisely targeted and dosed radiation is used to kill cancer cells left behind after surgery. This therapy is important to control the local growth of tumor. If the tumor has spread, radiation to the whole brain and spinal cord is important to treat ependymoma.
Chemotherapy - the role of anti-tumor medications in treating ependymoma is actively being studied. New agents are under investigation.
Follow-up care - to manage disease complications, to screen for early recurrence of tumor and to manage late effects of treatment, regular visits with physical exams, laboratory testing, and scans are routine follow-up. In addition to neurosurgeons, radiation oncologists, pediatric oncologists and neurologists, the endocrinologists, neuro-psychologists, alternative/complementary therapy specialists, school liaison and psychosocial personnel continue to serve as members of the neuro-oncology team.
Rehabilitation - speech, physical, and occupational therapists are also part of the neuro-oncology team, and may be involved during and after treatments.
Within the brain and posterior fossa, patients do best when their tumor can be completely removed surgically, and if high dose focal radiation therapy is given. For spinal cord ependymomas, a similar approach is used, but with lower radiation doses. A metastatic tumor (ependymoma that has spread) requires additional whole brain and spine radiation.
What is the expected outcome (prognosis) for ependymoma after treatment?
Ependymoma of the brain treated with complete resection and radiation to the tumor area can result in an approximately 50 percent cure rate. Spinal cord ependymomas are often easier to treat, and have an excellent prognosis. Metastatic, progressive or recurrent ependymoma is more difficult to cure.
 Craniopharyngioma
Craniopharyngioma
OVERVIEW:
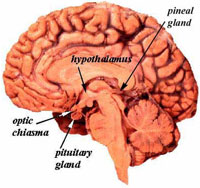
Craniopharyngiomas are benign brain tumors that arise near the pituitary gland and pituitary stalk and are typically both cystic and solid in structure. They occur most commonly in childhood and adolescence and in later adult life, after age 50. They account for 10-15% of sellar and suprasellar tumors (tumors that occur in and above the pituitary gland) and 50-60% of sellar and suprasellar tumors in children. They are usually not discovered until they impinge upon important structures around them, and are frequently quite large (over 3 cm) when detected. Although they are benign (not malignant) tumors, these tumors tend to become adherent to structures around the pituitary gland and stalk, including the optic nerves, optic chiasm, intracranial arteries and the brain itself. They are thought to arise from remnants of the craniopharyngeal duct or Rathke's pouch which are developmental structures related to the primitive gut. They are thought to be closely related to Rathke’s Cleft Cysts (RCCs).
SYMPTOMS:
Craniopharyngiomas can cause a variety of symptoms depending upon their location. If the tumor compresses the pituitary stalk or gland, the tumor can cause partial or complete pituitary hormone deficiency which may lead to growth failure, delayed puberty, loss of normal menstrual function or sexual desire, increased sensitivity to cold, fatigue, constipation, dry skin, nausea, low blood pressure, and depression. Pituitary stalk compression can also cause diabetes insipidus (DI), and increase prolactin levels causing a milky discharge from the breast (galactohhrea). If the tumor compresses the optic chiasm or nerves, then visual loss can result. Involvement of the hypothalamus, an area at the base of the brain, may result in obesity, increased drowsiness and temperature regulation abnormalities. Other symptoms especially with larger tumors may include personality changes, headache, confusion, and vomiting.
DIAGNOSIS:
The best means of visualizing a craniopharyngioma is with an MRI of the pituitary region. Many craniopharyngiomas will also be well seen on a CT scan especially since some are partially calcified (containing calcium deposits). A complete pituitary hormonal blood evaluation should also be performed. Other possible diagnoses to consider with a cystic pituitary mass is a cystic pituitary adenoma or an arachnoid cyst.
TREATMENT:
Surgery: The typical initial treatment for a craniopharyngioma is surgical removal by either the endonasal transsphenoidal approach or by a supra-orbital “eyebrow” craniotomy. The goal of surgery is to completely remove the tumor while improving vision and brain function. Because of their tendency to be adherent to the optic chiasm, other nerves and important blood vessels, complete tumor removal may not be possible in up to 50% of patients.
Radiosurgery (SRS) or Stereotactic Radiotherapy (SRT): With incomplete removal, stereotactic radiotherapy (SRT) or stereotactic radiosurgery (SRS), are typically used to prevent further tumor growth. Additionally, because of the tendency for craniopharyngiomas to recur, repeat MRIs or CT scans should be obtained at least every six months for the first 5 years after surgery or radiation therapy and then at least annually thereafter.
Hormonal Replacement Therapy: Many patients with a craniopharyngioma will develop pituitary hormonal deficits because of the tumor itself, surgery or as a consequence of radiotherapy. Such patients will require hormone replacement therapy such thyroid, cortisol, testosterone (men), estrogen (women) and/or DDAVP for diabetes insipidus. Because hormonal deficiencies can develop many years after radiation treatment, patients treated with radiation should have periodic hormonal evaluations throughout their lifetimes. Regular follow-up with an endocrinologist is recommended for all patients with a craniopharyngioma.
 Brain Stem Glioma, Central Nervous System
Brain Stem Glioma, Central Nervous System
Introduction
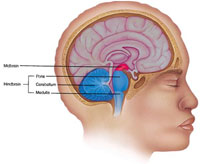
The brain stem connects the brain to the spinal cord. It is the lowest portion of the brain, above the back of the neck. The brain stem controls many of the body's basic functions, such as motor and sensory activity, coordination and walking, and heart and respiratory functions. It has three parts:
- The midbrain, which develops from the middle of the brain
- The medulla oblongata, which connects to the spinal cord
- The pons, which is located between the medulla oblongata and the midbrain
Most brain stem tumors develop in the pons. A glioma is a tumor that grows from a glial cell, which is a supportive cell in the brain.
Brain stem glioma is most often diffused (spread freely) through the brain stem by the time of diagnosis. This type of tumor is very aggressive. A small percentage of brain stem tumors are very localized or focal tumors. Focal tumors often are low-grade (the cells look close to normal) tumors, and behave in a more benign (less aggressive) fashion.
Brain stem glioma tends to occur in children between five and 10 years old. Most tumors grow in a part of the brain stem that can be difficult to perform surgery in, making brain stem glioma challenging to treat.
Risk Factors
A risk factor is anything that increases a person's chance of developing a disease, including cancer. There are risk factors that can be controlled, such as smoking, and risk factors that cannot be controlled, such as age and family history. Although risk factors can influence disease, for many risk factors it is not known whether they actually cause the disease directly. Some people with several risk factors never develop the disease, while others with no known risk factors do.
Doctors and researchers don't know what causes most childhood cancers. Some evidence indicates that genetic factors may play a role in a small percentage of brain stem gliomas. Genetic conditions associated with a higher risk of central nervous system (CNS) tumors include Li-Fraumeni syndrome, tuberous sclerosis, nevoid basal cell syndrome, and Turcot syndrome.
Symptoms
Children with brain stem glioma often experience the following symptoms. Sometimes, children with brain stem glioma do not show any of these symptoms. Or, these symptoms may be similar to symptoms of other medical conditions. If you are concerned about a symptom on this list, please talk to your child's doctor.
- Double vision or an inability to close the eyelids
- Drooping of the face
- Difficulty chewing and swallowing food
- Weakness in the arms and legs, clumsiness or wobbliness, and difficulty walking
- Difficulty talking
- Headache
- Vomiting
Diagnosis
Doctors use many tests to diagnose cancer and determine if it has metastasized (spread). Some tests may also determine which treatments may be the most effective. For most types of cancer, a biopsy is the only way to make a definitive diagnosis of cancer. However, biopsies are rarely used and are often specifically avoided in children with diffuse brain stem glioma because they do not influence treatment, and they can carry major risks. In addition, the diagnosis can generally be made by magnetic resonance imaging (MRI) alone (see below). Diffuse brain stem glioma is unlike most other types of tumors in this regard. For a focal tumor, a biopsy and surgical tumor removal may be considered. If a biopsy is not deemed possible, the doctor may suggest other tests that will help make a diagnosis. Imaging tests may be used to find out whether the cancer has metastasized. Your child's doctor may consider these factors when choosing a diagnostic test:Age and medical condition, The type of cancer, Severity of symptoms, Previous test results.
The following tests may be used to diagnose brain stem glioma:
Physical examination. A physical examination may include tests to determine brain function, reflexes, vision, and hearing of the child.
Computed tomography (CT or CAT) scan. A CT scan creates a three-dimensional picture of the inside of the child's body with an x-ray machine. A computer then combines these images into a detailed, cross-sectional view that shows any abnormalities or tumors. Sometimes, a contrast medium (a special dye) is injected into a vein to provide better detail. For a brain stem tumor, this test is generally insufficient to establish the diagnosis conclusively, and an MRI is required (see below).
Magnetic resonance imaging (MRI). An MRI uses magnetic fields, not x-rays, to produce detailed images of the body.
Biopsy. A biopsy is not generally done for the more common diffuse types of brain stem tumors. However, for focal tumors, it is often used to determine the type of cancer. If possible, a neurosurgeon (a specialist who operates on the head and brain) will remove a small piece of tissue from the brain. The doctor will examine the tissue under a microscope and look for cancer cells.
Treatment
Clinical trials are the standard of care for the treatment of children with cancer. In fact, more than 60% of children with cancer are treated as part of a clinical trial. Clinical trials are research studies that compare standard treatments (the best treatments available) with newer treatments that may be more effective. Cancer in children is rare, so it can be hard for doctors to plan treatments unless they know what has been most effective in other children. Investigating new treatments involves careful monitoring using scientific methods, and all participants are followed closely to track progress.
To take advantage of these newer treatments, all children with cancer should be treated at a specialized cancer center. Doctors at these centers have extensive experience in treating children with cancer and have access to the latest research. Many times, a team of doctors treats children with cancer. Pediatric cancer centers often have extra support services for children and their families, such as nutritionists, social workers, and counselors. Special activities for kids with cancer may also be available.
Three types of therapies can be used to treat brain stem glioma in children: radiation therapy, surgery, and chemotherapy. Sometimes, the treatments are used in combination.
Radiation therapy
Radiation therapy uses x-rays or other high-energy particles to kill cancer cells. Radiation therapy is the most common treatment for brain stem glioma.
Fatigue, drowsiness, nausea, vomiting, and headache are common side effects of radiation therapy. Because radiation therapy can sometimes interfere with the normal growth and development of the child's brain, the doctor may choose to treat the cancer in another way. To avoid or reduce the need for radiation treatment in young children, the doctor may use chemotherapy to shrink the tumor.
Chemotherapy
Chemotherapy uses drugs to kill cancer cells. Because it kills cancer cells throughout the body, it is called a systemic treatment.
Chemotherapy alone is not an effective treatment for brain stem glioma; however, in some cases, a doctor may use chemotherapy during or after radiation treatments.
Because chemotherapy attacks rapidly dividing cells, including those in normal tissues such as the hair, lining of the mouth, intestines, and bone marrow, children receiving chemotherapy may lose their hair, develop mouth sores, or have nausea and vomiting. Chemotherapy may lower the body's resistance to infection, lead to increased bruising and bleeding, and cause fatigue. These side effects can be controlled during treatment and usually go away after chemotherapy is completed. The severity of the side effects depends on the type and amount of the drug being given and the length of time the child receives the drug.
The medications used to treat cancer are continually being evaluated. Talking with your doctor is often the best way to learn about the medications you've been prescribed, their purpose, and their potential side effects or interactions with other medications. Learn more about your prescriptions through PLWC's Drug Information Resources, which provides links to searchable drug databases.
Surgery
Surgery is used to treat brain stem glioma only when the tumor's appearance on an MRI scan is focal, thus suggesting it may be possible to remove the cancer without damaging the brain, such as when a tumor grows out from the brain stem. For most children with diffuse types of brain stem gliomas, surgery is not necessary or possible because of the location of the tumor and the risk involved.
Recurrent brain stem glioma
Treatment for recurrent brain stem glioma (cancer that comes back after treatment)depends on two factors:
The type of tumor
The type of treatment the child received for the original tumor
Depending on individual circumstances, the doctor may recommend either surgery or chemotherapy.
Side Effects of Cancer and Cancer Treatment
Cancer and cancer treatment can cause a variety of side effects; some are easily controlled and others require specialized care. Below are some of the side effects that are more common to brain stem glioma and its treatments. For more detailed information on managing these and other side effects of cancer and cancer treatment, visit the PLWC Managing Side Effects section.
Anemia. Anemia is common in people with cancer, especially those receiving chemotherapy. Anemia is an abnormally low level of red blood cells (RBCs). RBCs contain hemoglobin (an iron protein) that carries oxygen to all parts of the body. If the level of RBCs is too low, parts of the body do not get enough oxygen and cannot work properly. Most people with anemia feel tired or weak. The fatigue (tiredness) associated with anemia can seriously affect quality of life and make it more difficult for patients to cope with cancer and treatment side effects.
Fatigue. Fatigue is extreme exhaustion or tiredness, and is the most common problem that people with cancer experience. More than half of patients experience fatigue during chemotherapy or radiation therapy, and up to 70% of patients with advanced cancer experience fatigue. Patients who feel fatigue often say that even a small effort, such as walking across a room, can seem like too much. Fatigue can seriously impact family and other daily activities, can make patients avoid or skip cancer treatments, and may even impact the will to live.
Hair loss (alopecia). A potential side effect of radiation therapy and chemotherapy is hair loss. Radiation therapy and chemotherapy cause hair loss by damaging the hair follicles responsible for hair growth. Hair loss may occur throughout the body, including the head, face, arms, legs, underarms, and pubic area. The hair may fall out entirely, gradually, or in sections. In some cases, the hair will simply thin-sometimes unnoticeably-and may become duller and dryer. Losing one's hair can be a psychologically and emotionally challenging experience and can affect a patient's self-image and quality of life. However, the hair loss is usually temporary, and the hair often grows back.
Mouth sores (mucositis). Mucositis is an inflammation of the inside of the mouth and throat, leading to painful ulcers and mouth sores. It occurs in up to 40% of patients receiving chemotherapy treatments. Mucositis can be caused by a chemotherapeutic drug directly, the reduced immunity brought on by chemotherapy, or radiation treatment to the head and neck area.
Nausea and vomiting. Vomiting, also called emesis or throwing up, is the act of expelling the contents of the stomach through the mouth. It is a natural way for the body to rid itself of harmful substances. Nausea is the urge to vomit. Nausea and vomiting are common in patients receiving chemotherapy for cancer and in some patients receiving radiation therapy. Many patients with cancer say they fear nausea and vomiting more than any other side effects of treatment. When it is minor and treated quickly, nausea and vomiting can be quite uncomfortable but cause no serious problems. Persistent vomiting can cause dehydration, electrolyte imbalance, weight loss, depression, and avoidance of chemotherapy.
Nervous system disturbances. Nervous system disturbances can be caused by many different factors, including cancer, cancer treatments, medications, or other disorders. Symptoms that result from a disruption or damage to the nerves caused by cancer treatment (such as surgery, radiation treatment, or chemotherapy) can appear soon after treatment or many years later. See Managing Side Effects: Nervous System Disturbances for the most common symptoms.
Sleeping problems: hypersomnia, somnolence syndrome, and nightmares. Hypersomnia, also called somnolence, excessive daytime sleepiness, or prolonged drowsiness, is a condition characterized by excessive sleeping or the inability to maintain wakefulness when desired. Somnolence syndrome is a type of hypersomnia associated with cranial radiation therapy (radiation treatment to the head) in children. Symptoms of somnolence syndrome include excessive drowsiness, prolonged periods of sleep (up to 20 hours a day), headaches, low-grade fever, nausea and/or vomiting, and irritability. Nightmares are vivid, frightening dreams that usually cause the dreamer to wake up able to remember part or most of the nightmare. Most people have nightmares from time to time, but the frequency or vividness of nightmares can increase after a cancer diagnosis and during cancer treatment. Possible causes of hypersomnia include some brain cancers in adults (for example, ependymoma or meningioma); some childhood central nervous system (CNS) cancers (for example, brain stem glioma, cerebellar astrocytoma, medulloblastoma); some secondary brain tumors (brain metastases); some chemotherapeutic drugs (for example, teniposide [VM-26], pegaspargase [Oncaspar], thalidomide [Thalomid]); and other prescription and over-the-counter medications (for example, some antidepressants, antinausea medications, opioid pain killers, sedatives, antihistamines, sleeping pills).
After Treatment
The child's follow-up care plan and the long-term risks following therapy depend on several factors, such as the type of tumor and its location, the age of the child, and the type of treatment. For example, craniospinal radiation therapy can cause cognitive and endocrine symptoms over time, although the severity can vary greatly depending on the dose administered and the age of the child. Similarly, the risks and potential side effects of surgery vary dramatically, depending on the location and characteristics of the tumor. Likewise, the risks of chemotherapy and the likelihood of secondary cancers are strongly influenced by the drugs used and their doses. For each of these issues, it is important to discuss the specific aspects of the tumor and the options for treatment with the neurosurgeons and neuro-oncologists that are involved in the child's care.
 Spinal Tumors
Spinal Tumors
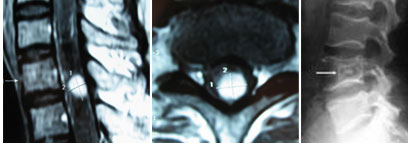
A Spinal tumor - a cancerous or noncancerous growth that develops with the cervical (neck), thoracic (midback) or lumbosacral (lowback) regions or near the spinal cord or bones of the spine. They may be primary originating from the spinal cord or metastatic originating elsewhere (eg: lung, breast etc)
Anatomy of Spine
The spine is composed of individual bones (vertebrae) stacked one on top of the other in a column. Each vertebra possesses a cylindrical body, which participates in weight bearing and an arch of bone (laminae and spinous processes) which protects the spinal cord and its coverings. The bony arch is connected to the body by two small columns of bone (pedicles). The circular canal between the body, arch, and pedicles houses the spinal cord and is called the spinal canal.
The spinal cord is contained within the spinal canal and is covered by a layer of connective tissue, the dura mater. Tumors which are located outside the dura are called extradural. These are usually metastatic tumors and most often arise in the vertebrae themselves. Tumors arising inside the dura, but outside the actual substance of the spinal cord are termed intradural-extramedullary. These are usually nerve sheath tumors or meningiomas. Tumors arising within the substance of the spinal cord itself are called intramedullary tumors. These are usually astrocytomas or ependymomas. Different types of tumors often behave differently and require different treatments.
 Causes of Spinal Tumors
Causes of Spinal Tumors
Primary spinal cord tumors may be extramedullary (occurring outside the spinal cord) or Intramedullary (occurring within the cord itself).
Extramedullary tumors may be intradural (meningiomas and schwannomas) which account for 60% of all primary spinal cord neoplasms or extradural (metastatic tumors like from breasts, lungs, prostate, leukemia or lymphomas) which account for 25% of these neoplasms. Intramedullary tumors or gliomas (astrocytomas or ependymomas) are comparatively rare accounting for only about 10% of tumors. Spinal tumors are rare compared with intracranial tumors (ratio 1:4). They occur with equal frequency in men and women with the exception of meningiomas which occur most often in women. Spinal cord tumors can occur anywhere along the length of cord or its roots
Symptoms of Spinal Tumors
- Neck and back pain are common presenting symptoms of spinal cord tumors.
- The pain is often present at night and is worsened with physical activity.
- Loss of sensation or weakness especially in legs.
- Difficulty in walking sometimes leading to falls.
- Decreased sensitivity to pain, heat and cold.
- Loss of bowel and bladder function.
- Paralysis that may occur in varying degrees and n different parts of body depending on which nerves are compressed.
Diagnosis of Spinal Tumors
Diagnosis of spinal tumors begins with history and physical examination
- Plain X-Rays
- Spinal Magnetic Resonance Imaging (MRI)
- CT Scan
- Myelogram
- Biopsy- whether the tumor is benign or malignant
Treatment of Spinal Tumors
Non Surgical Treatment of Spinal Tumors
DRUGS-because surgery and radiation therapy as well as tumors themselves can cause inflammation inside the spinal cord, doctors sometimes prescribe corticosteroids to reduce swelling either following surgery or during treatment.
Surgical Treatment of Spinal Tumors
Surgical options for the treated of spine tumors vary from complete to partial removal. Surgical stabilization of the spine may be necessary as a result of instability caused by tumor itself or the surgery to remove it. This may be done by surgery approach from the front or back of spine. This may involve going through the neck, chest or abdomen. Newer techniques and instruments allows that were once inaccessible. The high powered microscopes used in microsurgery for instance make it easier to distinguish tumors from healthy tissue. The typical hospital stays after surgery to remove a spinal tumors range from approximately 5 to 10days
Radition therapy- This therapy is used following an operation to eliminate the remnant of tumors that can't be completely removed or to treat inoperable tumors.