|
Appendicitis
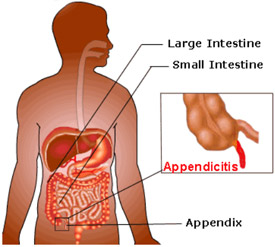 Appendicitis is diagnosed when there is an inflammation of the appendix. The appendix is a small finger-shaped pouch attached to the large intestine and is generally found on the lower right side of the abdomen. This organ of body does not have any function. Appendicitis creates a medical emergency and doctors have to perform immediate surgery to remove the appendix. If treatment is not given at crisis time, inflamed appendix will ultimately burst, or perforate, spilling infectious materials into the abdominal cavity. This can lead to peritonitis, a severe inflammation of the abdominal cavity's lining that can be deadly unless it is treated rapidly with strong antibiotics. Sometimes a pus-filled abscess that is an infection that is walled off from the rest of the body forms outside the inflamed appendix. An abscessed appendix is an emergency situation. But it can not be identified without surgery. Due to these facts, cases of appendicitis require surgery. Appendicitis is diagnosed when there is an inflammation of the appendix. The appendix is a small finger-shaped pouch attached to the large intestine and is generally found on the lower right side of the abdomen. This organ of body does not have any function. Appendicitis creates a medical emergency and doctors have to perform immediate surgery to remove the appendix. If treatment is not given at crisis time, inflamed appendix will ultimately burst, or perforate, spilling infectious materials into the abdominal cavity. This can lead to peritonitis, a severe inflammation of the abdominal cavity's lining that can be deadly unless it is treated rapidly with strong antibiotics. Sometimes a pus-filled abscess that is an infection that is walled off from the rest of the body forms outside the inflamed appendix. An abscessed appendix is an emergency situation. But it can not be identified without surgery. Due to these facts, cases of appendicitis require surgery.
There is no specific age when appendicitis can occur. But medical data shows that it is uncommon under age 2 and most common between ages 10 and 30. Patients have appendicitis when the appendix becomes blocked, often by stool, a foreign body, or cancer. Obstruction may also occur from infection, since the appendix swells in reaction to any infectivity in the body.
Symptoms
Patient suffering from Appendicitis exhibit many symptoms that include: Dull pain near the navel or the upper abdomen that becomes intense as it moves to the lower right abdomen. This is considered as a first sign of appendicitis. Patients feel nausea and/or vomiting soon after abdominal pain begins. There is loss of appetite, abdominal swelling, fever range from 99° F to 102° F, failure to pass gas almost half the time. Other symptoms are sharp pain anywhere in the upper or lower abdomen, back or rectum. Patients feel pain in passing urine. Patient vomits that go before the abdominal pain. Patients have severe cramps, and complain for constipation or diarrhea with gas. It is advised to patients that they must contact doctor if they have pain with above symptoms. They must not do experiment by eating something, having drinks, or take any pain killer, antacids, laxatives, or heating pads, which can cause an inflamed appendix to rupture. Visit to doctor immediately for timely diagnosis and proper treatment that is very important to get relieve from disease.
Diagnosis
Diagnosis of appendicitis can be difficult because patients show similar symptoms that match with other illness. For example, patients who suffer from gallbladder problems, bladder or urinary tract infection, Crohn's disease, gastritis, intestinal infection and ovary problems show parallel symptoms. Patient must visit expert medical professional for correct diagnosis. Some tests are frequently done for the diagnosis of appendicitis. There are abdominal exam to detect inflammation, urine test to rule out a urinary tract infection, rectal exam, blood test to observe if body is fighting infection, CT scans and/or ultrasound
Treatment
For the treatment of appendicitis, surgery is done to remove the appendix, which is termed as an appendectomy in medical language. It is the normal treatment for appendicitis. Antibiotics are prescribed before an appendectomy to fight possible peritonitis. When surgery is done, patient is given general anesthesia and the appendix is removed through a 4-inch incision or by laparoscopy. If Patients have peritonitis, the abdomen is also irrigated and drained of pus. After 12 hours of surgery, patients may become conscious. Patients have to be hospitalized for sometime and they can perform normal activities in 2 to 3 weeks. If a laparoscope technique is used to operate the appendix, the cut is smaller and patients recover speedily.
It is very important to take care after operation. After an appendectomy, if patients complain for uncontrolled vomiting, increased pain in abdomen, dizziness/feelings of faintness, blood in vomit or urine, increased pain and redness in cut, fever and pus in the wound, they should immediately call doctor to avoid major complications. All people must understand that appendicitis can not be prevented. It can be said that appendicitis is less common in people who take high fibrous diet such as fresh fruits and vegetables.
Alimentary Tract Obstruction
Obstruction of the alimentary tract (tubes of digestion extending from the mouth to the anus) is characterized by four cardinal symptoms: abdominal distention (an abdomen that becomes large and appears swollen), bilious vomiting (due to bile in the stomach), maternal polyhydramnios (excess amniotic fluid in the amniotic sac, greater than 2,000 ml) before birth, failure to pass meconium (dark green or black sticky excretion passed via the newborn's rectum) in the first 24 hours of life
Esophageal Atresia and Tracheoesophageal Fistula
This is a congenital deformity of the esophagus (the tube that passes food from the mouth to the stomach). Symptoms include severe respiratory distress (the neonate cannot breathe) and excessive salivation. Other clinical signs include cyanosis (bluish discoloration of the skin due to oxygen deprivation), choking, and coughing.
Anorectal Anomalies
There are many different types of anorectal anomalies common to male and female neonates, as well as deformities that are gender-specific since involvement of genitalia can occur. The surgery for these cases is complicated, and must be performed by an experienced pediatric surgeon. Complications of these procedures could result in permanent problems.
Necrotizing Enterocolitis (NEC)
NEC affects 12% of patients admitted to a neonatal intensive care unit. It is a life-threatening illness characterized by abdominal distention, bilious vomiting, lethargy, fever, occult (not obvious) or gross (clearly seen) rectal bleeding. Additionally, affected patients may exhibit signs of hypothermia (temperature less than 96.5°F or 35.8°C), bradycardia (slow heart rate), abdominal mass (felt during palpation), oliguria, jaundice, and episodes of breathlessness (apnea). Survival of NEC surgery can be expected for 6070% of patients.
Abdominal Wall Defects
Omphalocele is a defect that involves protrusion of abdominal contents into an external sac. This disorder occurs in one per 5,000 births. More than 50% of omphalocele patients have serious genetic deformities involving these body systems: cardiovascular (heart), musculoskeletal (muscle and bones), genitourinary (genital and bladder systems), and central nervous (brain and spinal cord). The overall survival rate for infants with omphalocele varies, and depends on defect size, other associated genetic abnormalities, and age of newborn. (Many infants with omphalocele are premature.) Approximately 33% of patients with omphaloceles do not survive.
Congenital Diaphragmatic Hernia (CDH)
CDH can be diagnosed by the fourth month of pregnancy via ultrasound studies. Of the infants with congenital diaphragmatic hernia (CDH), 4466% have other congenital abnormalities as a result of developmental malformations. Anatomically, patients with CDH have a defect in development that allows a communication between the chest and abdomen. Through this defect, the abdominal contents enter the lung cavity and interfere with normal lung development. The incidence is approximately one per 2,200 live births, and males are more commonly affected than females. Usually the infants are full-term, and the defect occurs on the left side in the majority88%of patients.
Treatment is extensive, and usually requires three major areas:
- Stabilization of patient and preoperative preparation
- Operative treatment
- Postoperative respiratory, metabolic, circulatory, and nutritional supportive measures
Postoperatively, the infant is monitored in the neonatal intensive care setting. The postoperative period is more critical if a lung is severely underdeveloped.
Pyloric Stenosis (PS)
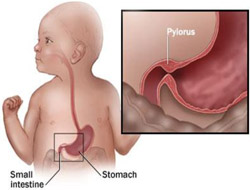 Pyloric stenosis is an obstruction in the intestine due to a larger-than-normal size of the muscle fibers of the pylorus (lower stomach opening). Pyloric stenosis is a common hereditary condition that affects males more than females, and occurs in one per 750 births. The typical symptoms include a progressive, often projectile, vomiting after attempted feedings. The gastric vomitus (bloody in 80% of patients) usually begins during the second and third week of life, and increases in force and frequency. Typically, the infant fails to gain weight, and the number of bowel movements and rate of urination decreases. Pyloric stenosis is an obstruction in the intestine due to a larger-than-normal size of the muscle fibers of the pylorus (lower stomach opening). Pyloric stenosis is a common hereditary condition that affects males more than females, and occurs in one per 750 births. The typical symptoms include a progressive, often projectile, vomiting after attempted feedings. The gastric vomitus (bloody in 80% of patients) usually begins during the second and third week of life, and increases in force and frequency. Typically, the infant fails to gain weight, and the number of bowel movements and rate of urination decreases.
Physical examination is usually helpful in establishing a diagnosis. Palpation of the enlarged muscle fibers can be felt as an olive-shaped mass located in the midline approximately one-third to one-half of the distance from the umbilicus to the xiphoid (end of the breast bone), when the stomach is empty.
Careful abdominal examination and palpation can usually identify the pyloric mass in 85% of cases.
Gastroesophageal Reflux
Gastroesophageal reflux (GER) is a common disorder in infancy, and usually disappears by the baby's first birthday. The largest group of patients with clinically significant GER are those who have neurologic impairment. Symptoms often include vomiting, repeated lung infections (from aspirating gastric contents during regurgitation of foodstuffs), and delayed gastric emptying. The success rate with infants who have procedures necessary to correct GER is over 90%.
Meckel's Diverticulum
Meckel's diverticulum occurs in approximately 2% of the U.S. population. The diverticulum is an outgrowth of intestine is located in a portion of the intestines called the ileum. Symptoms of obstruction are more often observed in infants, and bleeding is more common in patients after age four.
Intestinal Polyps
Juvenile polyps are usually present between the ages of four and 14 years, and tend to be inflammatory. The most common symptom of intestinal polyps is rectal bleeding, which is commonly due to a solitary polyp (80% of cases). Diagnosis can be done by proctosigmoidoscopy, which allows visualization of 85% of polyps.
Inflammatory Bowel Diseases
Some cases (approximately 25%) of inflammatory bowel disease are found in persons younger than 20 years of age. Two types can occur, Crohn's disease and ulcerative colitis.
The diagnosis of inflammatory bowel disease is usually based on presenting clinical symptoms, laboratory analysis results, endoscopic appearance, and radiologic findings. Approximately 5060% of patients have bloody diarrhea, severe cramping, abdominal pain, and urgency.
Crohn's Disease
The symptoms of Crohn's disease includes cramping abdominal pain, diarrhea, and strictures (constriction) resulting from bowel obstruction. Removal of diseased portions in children with Crohn's disease may be temporarily beneficial, but recurrence after surgical removal occurs in about 50% of cases within four years. Chronic symptoms may remain into adult life, making long-term follow-up essential.
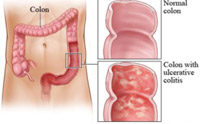 Ulcerative Colitis Ulcerative Colitis
Ulcerative colitis is limited to the colon. A surgical procedure known as colectomy is curative, and indicated for intractable disease (64% of patients). Colectomy is the removal of the entire colon, or the inflamed part of it.
Neonatal Jaundice
Neonatal jaundice is common, and results from an immature system not capable of some basic biochemical reactions. Food intake can help speed these reactions, which usually resolves the condition within seven to 10 days. Jaundice that persists for over two weeks is abnormal, and could be caused by over 30 possible disorders.
Biliary Atresia
Biliary atresia is a disease that causes inflammation of the ducts within the biliary system, resulting in fibrosis of these ducts. The incidence of biliary atresia is one per 15,000 live births, and is more common in females. Time is critical, and most patients must have surgery by two months of life. Approximately 2530% of patients who receive early operative intervention have long-term successful outcomes. Some patients may require liver transplantation, and 8590% of these patients survive.
Cholelithiasis
Gallbladder obstruction in infants and young children is usually caused by pigmented (colored) stones resulting from blood disorders. Removal of the gallbladder (laparoscopic cholecystectomy) is the treatment of choice.
Trauma
Accidents are the leading cause of death in children between the ages of one and 15 years, and accounts for 50% of all deaths in the pediatric age group. More than half of these deaths are due to motor vehicle accidents, followed by falls, bicycle injuries, drowning, burns, child abuse, and birth trauma. Head trauma is the single most common organ associated with traumatic death. Within recent years, the number of fatalities related to the use of firearms and violence has increased.
More than 20 million children each year sustain injuries requiring treatment. These injuries account for 100,000 cases of permanent pediatric disability. Response to trauma in pediatric patients is significantly different from older patients. Pediatric patients require special attention concerning temperature regulation, blood volume, metabolic rate and requirements, and airway maintenance. Other special pediatric considerations include response to stress, communication difficulties, psychological trauma, a different pediatric trauma score system, smaller airway diameter, and increased risk of aspirating gastric contents (which could cause pneumonia). Pediatric trauma patients should have access to appropriate pre-hospital transportation, and must receive medical attention in a pediatric trauma center capable of providing the complex level of care necessary for serious pediatric trauma situations.
Neck Masses
Neck masses during infancy and childhood may be caused by tumors or infections, or they may be congenital. Lymphadenitis is an infection of a lymph node that becomes enlarged and tender. Most cases are resolved by treating the primary source of infection (i.e., middle ear infection and tonsillitis). Some inflamed nodes may require an incision and drainage of infection.
Hernias
Inguinal Hernia and Hydrocele
Inguinal (groin) hernia is the most frequent disorder requiring surgery in the pediatric age group. Clinically, a right-sided inguinal hernia is more common in males (60% of cases), and there is a familial tendency. The incidence is higher in full-term infants (3.55%). Full-term infants and older children (without underlying diseases) can receive surgical repair in an outpatient setting. An inguinal hernia may result in herniation of the scrotum, and a communicating hydrocele (hernia with a small connection to the peritoneal cavity).
Umbilical Hernia
Umbilical hernia is a defect of the umbilical ring, and is more common in females and African American children. Spontaneous involution occurs in 80% of cases. Larger defects may be observed for several years without complications, and their spontaneous resolution is possible. If the umbilical hernia persists, patients may develop feeding intolerance, pain, and local skin breakdown.
Undescended Testes
Undescended testes are observed in 12% of full-term males. Approximately 30% of preterm males may have an undescended testis. Undescended testis in premature infants may descend by the first year of life, and observation is often the treatment during that time.
Tumors: Nephroblastoma
Wilm's tumor (nephroblastoma) is a tumor in the kidneys that forms during embryonic development. The tumor is due to a genetic abnormality; and approximately 80% of children are diagnosed between one and five years of age. In about 7595% of cases, the patient has an abdominal mass that is detected by a parent during bathing. Blood in the urine (hematuria) occurs in 1015% of cases, and high blood pressure (hypertension) is present in 2025% of cases.
Hypertension is the result of the tumor compressing the kidney in a specific area, causing it to release a chemical called renin, which elevates blood pressure. During physical examination, the Wilm's tumor is a smooth, round, hard, nontender flank mass. The treatment of Wilm's tumor depends on its stage, and may include surgery, chemotherapy, or radiotherapy.
Scoliosis
Scoliosis is a deformity of the spine which causes a sideways S- or C-shaped curvature to develop over time. Many of us have slight deviations in our spines, but medical professionals tend to wait until the curvature is past ten degrees to diagnose scoliosis. A ten degree spinal deviation is not easily detectable -- it may only appear as a slight droop in one shoulder or a slightly uneven waistline. Some scoliosis sufferers can have as much as a thirty degree deviation without noticeable pain. Scoliosis with a C-curve is more common than an S-curve. The S shape forms as the spine tries to correct the original C-shape deviation.
Some sources suggest that as many as 25% of the general population has experienced some form of undiagnosed scoliosis during childhood, but the most severe form only affects 3% or so. Most incidents of scoliosis are considered ideopathic, or from an unknown cause.
Girls, especially those in the prepubescent growth stage, are much more likely to contract scoliosis than boys. This may be connected to the earlier growth spurts experienced by girls between the ages of 10 and 14. Adult onset of scoliosis is rare, but not completely out of the question. Neuromuscular conditions such as MS or extremely poor posture can lead to a pronounced curvature of the spine.
The good news is that most scoliosis sufferers either outgrow the condition or undergo successful corrective surgery. Some orthopedists will use a body brace resembling a corset on scoliosis patients who are still growing. The brace is meant to encourage a straighter path for the developing spine to follow, but it won't necessarily correct any existing curvature. A common surgical practice for severe scoliosis involves fusing several vertebrae together to correct the patient's posture and prevent further twisting. Chiropractic treatments such as spinal manipulations do not appear to have very high success rates.
Scoliosis may sound more ominous than it actually is. Unless the degree of curvature is very pronounced, many children and adults may never realize anything is out of order. Many schools offer free scoliosis screenings for younger students, with any positive findings reported directly to parents. A family physician may also be able to test young patients for any lateral deviations in the spine. If the condition is discovered early and corrective action is taken, the effects of scoliosis can be controlled if not cured.
Cerebral palsy
While many infants are born worldwide with cerebral palsy every year, doctors and researchers alike do not know the genetic factors that may lead to this condition. While some researchers believe cerebral palsy can be present due to genetics, other research indicates cerebral palsy can be the effect of babies born to alcoholic or drug addicted mothers. Moreover, if a problem during the child's birth prevents the flow of oxygen to the brain, cerebral palsy can be a likely result. Cerebral palsy itself in a coverall term used to describe any number of medical conditions which afflict infants with the inability to control muscle movement. Cerebral palsy can usually be diagnosed by the time a child reaches 18 months due to the child's inability to be able to perform the standard motor skills associated with growing infants, such as sitting, reaching for toys, and walking. The conditions do not generally deteriorate with the passing of the years; rather they limit the activities a cerebral palsy victim can undertake.
Research indicates that cerebral palsy comes in many different forms. Spasticity is the term given to individuals who are unable to control their muscle movement. Someone afflicted with hemiplegia cannot control the muscles of an arm and a leg on the same side of the body. Quadriplegiacs have difficulty controlling and using all four limbs. Individuals who suffer from cerebral palsy can have a wide range of differences. One may have motor control issues that are hardly noticeable while another may suffer from extreme conditions which may, for instance, inhibit the way they walk or use their hands to eat.
There is no known cure for the many types of cerebral palsy. Doctors and therapists have designed a number of physical therapy programs designed to massage and relax the muscles of palsy victims. Lawyers have brought in a number of huge personal injury verdicts representing cerebral palsy victims when the lawyers are able to demonstrate that the palsy was brought upon as a result of the doctor's negligence while delivering the new born
Fetal surgery
Fetal surgery is any surgical procedure performed before the baby is born, while still in utero. Fetal surgery frequently allow surgeons to intervene early, before health issues or birth defects become more ominous. Certain birth defects may be exacerbated by the labor and delivery event and may even progress so quickly after birth as to cause extreme disability or death.
A condition called myelomeningocele, or spina bifida, is a birth defect where the spine does not close properly during fetal development. When this occurs, the spinal cord may be exposed or protrude through an open area in the lower portion of the back. If spina bifida fetal surgery is not performed, complications, such as neurological problems, paralysis, fluid in the brain, and bladder and bowel problems, may occur.
Typically, open fetal surgery is performed if fetal laser surgery, or endoscopic surgery, is not an option. Fetal surgery generally entails an incision being made through the mother's abdomen and part of the uterus being removed from the abdominal cavity. After a portion of the uterus is removed from the abdomen, often the amniotic fluid is then drained and kept warm for replacement when the procedure is completed. An incision is then made in the uterus, allowing the surgeon to perform the procedure on the fetus.
Generally, once a birth defect is discovered, doctors determine if fetal surgery will be an appropriate intervention. Fetal surgery is usually reserved for only the most extreme conditions that are likely to cause death or profound disability. If fetal surgical intervention is deemed appropriate, the parents, surgical team and other health care providers will meet to discuss the procedure.
Prior to the surgery, a steroid may be given to the patient to hasten fetal lung development. Next, a comprehensive physical examination will be done. Typically, a fetal monitor will be put in place to monitor the fetal heart rate and maternal uterine contractions. The maternal patient will not be allowed to eat or drink after midnight on the day of the surgery, and she will sign a consent form. Blood tests, called typing and cross matching, may be performed in case a blood transfusion is needed.
Recovery from fetal surgery typically takes up to ten days. The maternal patient will be watched closely for signs of premature labor; the physician may also recommend bed rest to decrease the risk
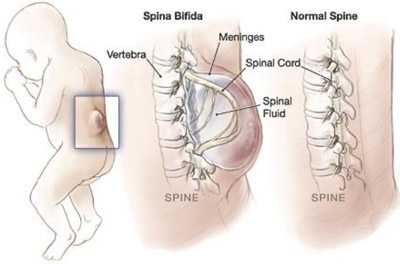 Spina bifida Spina bifida
Spina bifida describes varying birth defects caused by incomplete formation of the spine in utero. Along with problems associated directly with movement originating from the spine, spina bifida often causes permanent nerve damage to the areas affected. Though damage to the spine may be surgically corrected, nerves are generally not repairable and may impair brain function and movement.
Part of the spine may be exposed to the outside, and noticed at birth. Surgery is generally undertaken to close the spine and to place skin grafts over areas where the spine is exposed. Movement difficulties depend upon which area of the spine is affected.
For example, spina bifida in the lumbar region, the area between the abdomen and pelvis, tends to affect the legs, feet and knees. Usually those with lumbar malformations cannot walk or stand.
Spina bifida is categorized by location and severity. Three forms exist and they are: spina bifida cystica, spina bifida occulta, and meningocele. Spina bifida cystica is the most severe and difficult form. The spinal cord is open and may have been totally improperly formed. Brain function and movement are significantly affected, with many children fully or partially paralyzed. Fluid in the brain, hydrocephalus, is also a frequent occurrence requiring a shunt to reduce fluid.
Some studies indicate that fetal surgery may help reduce impairment caused by spina bifida cystica. Studies of unborn children with this type of spina bifida show that nerve damage worsens as the pregnancy progresses. There are several clinical trials now underway to evaluate the benefit of early closure of the spine to reduce symptoms after birth. These trials are still new, as is the ability to perform surgery on an unborn child. However, preliminary results look promising.
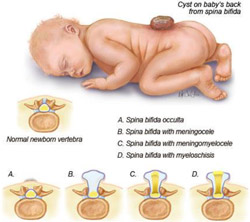 Spina bifida occulta is one of the least damaging types. The spine is not exposed at birth, and many may grow up completely unaware of their condition. Pain in the legs tends to manifest in adults who are in their 30s and 40s. Some people may be diagnosed earlier if the hips, knees or legs are deformed. Treatment usually revolves around closing the very small fracture or opening of the spine. Nerve damage, however, is usually permanent, though pain may be reduced. Spina bifida occulta is one of the least damaging types. The spine is not exposed at birth, and many may grow up completely unaware of their condition. Pain in the legs tends to manifest in adults who are in their 30s and 40s. Some people may be diagnosed earlier if the hips, knees or legs are deformed. Treatment usually revolves around closing the very small fracture or opening of the spine. Nerve damage, however, is usually permanent, though pain may be reduced.
Meningocele spina bifida usually looks the worst but has the best outcome for treatment. Skin may not have formed over the spine. The meninges, or membranous tissue of the spine are usually pushed through the skin causing a large cyst to form on the back. Though these tissues may be damaged somewhat, the nerves are usually not damaged. Surgery places the meninges back into the spine, and frequently results in an excellent outcome.
Not all causes for spina bifida are known. However, studies in the 1990s concluded that taking folic acid daily prior to pregnancy reduces risk significantly. Usually spina bifida begins with malformation of the neural tube, forming in the fourth week of pregnancy, so folic acid must be taken prior to conception to be effective.
Many early tests can scan for spina bifida and other neural tube defects. Amniocentesis can show evidence of spina bifida and other birth defects, and is usually performed between gestational weeks 14 and 16. Chronic villus sampling may also give much earlier detection, yet the results are somewhat disputed and may not always be accurate. Both tests carry some risks to the unborn child. Where a mother has already given birth to a child with spina bifida, risk may be slightly increased. Most obstetricians recommend both prenatal testing of the above types and genetic counseling.
Fetal surgery and increased understanding of spina bifida may help to eradicate its damage and its existence. Those affected may have significant impairment and challenges trying to live in a world not adjusted for those with disabilities. It is hoped that more study in this area will help future generations of children avoid spina bifida in any form.
|