|
Cardiac
Patent Ductus Arteriosus (PDA)
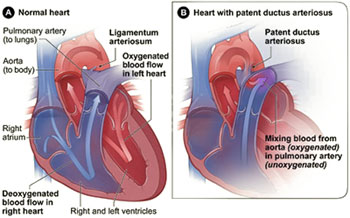 Patent ductus arteriosus (PDA) is a Congenital defect in which the temporary blood vessel connecting the left pulmonary artery to the aorta in the fetal heart fails to close after birth. In the fetal heart, blood bypasses the lungs and gets oxygen from the placenta. But when the newborn's lungs take over at birth, the body stops producing the chemicals that keep the ductus arteriosus open, and it closes naturally. Patent ductus arteriosus (PDA) is a Congenital defect in which the temporary blood vessel connecting the left pulmonary artery to the aorta in the fetal heart fails to close after birth. In the fetal heart, blood bypasses the lungs and gets oxygen from the placenta. But when the newborn's lungs take over at birth, the body stops producing the chemicals that keep the ductus arteriosus open, and it closes naturally.
If the ductus arteriosus fails to close completely, the baby has PDA While this problem is rare, it is sometimes associated with mothers who have had German measles (rubella) during pregnancy and with infants born before their due date (prematurely). The result of this defect is that too much blood travels to the lungs. The severity of the problem depends on how large the opening is and how prematurely the baby was born.
What Causes Patent Ductus Arteriosus?
The cause of patent ductus arteriosus (PDA) is not known. Genetics may play a role. A defect in one or more genes could prevent the ductus arteriosus from closing normally after birth.
PDA is more common in :
- Premature infants (babies born too early)
- Infants with genetic abnormalities such as Down syndrome
- Infants whose mother had German measles (rubella) during pregnancy
What Are the Signs and Symptoms of Patent Ductus Arteriosus?
Signs and symptoms may include :
- Fast breathing, working hard to breathe, or shortness of breath, or in the case of a premature infant, need for increased oxygen or ventilatory support
- Poor feeding and poor weight gain
- Tiring easily
- Sweating with exertion (such as while feeding)
How Is Patent Ductus Arteriosus Diagnosed?
In full-term infants, a patent ductus arteriosus (PDA) usually is first suspected when the baby's doctor hears a heart murmur during a regular checkup. If a PDA is large, the infant may also develop symptoms of volume overload and increased blood flow to the lungs. When a PDA is small, it may not be diagnosed until later in childhood. Once a PDA is suspected, a consultation with a pediatric cardiologist will be arranged. A pediatric cardiologist is a doctor who specializes in diagnosing and treating heart problems in children.
In premature babies (babies born too early) with PDA, the physical signs that are seen in full-term babies, such as heart murmur, may not be present. Doctors may suspect a PDA in premature babies who develop breathing difficulties soon after birth. Doctors use tests such as echocardiography to look for PDA in premature babies with breathing problems.
Tests for Patent Ductus Arteriosus
Two painless tests are used to diagnose a PDA
Echocardiogram :- This test, which is harmless and painless, uses sound waves to create a moving picture of your baby's heart. During an echocardiogram, reflected sound waves outline the heart's structure completely. The test allows the doctor to clearly see any problem with the way the heart is formed.
EKG (electrocardiogram): - This test records the electrical activity in the heart. In the case of a PDA, it can show: Enlargement of the heart chambers, Other subtle changes that can suggest the presence of a PDA
Treatment for patent ductus arteriosus
Specific treatment for PDA will be determined by your child's physician based on :
- Your child's age, overall health, and medical history
- Extent of the disease
- Your child's tolerance for specific medications, procedures, or therapies
- Expectations for the course of the disease
- Your opinion or preference
Post-procedure care for your child
Cath lab PDA repair/closure procedure : - When the procedure is complete, the catheter(s) will be withdrawn. Several gauze pads and a large piece of medical tape will be placed on the site where the catheter was inserted to prevent bleeding. In some cases, a small, flat weight or sandbag may be used to help keep pressure on the catheterization site and decrease the chance of bleeding. If blood vessels in the leg were used, your child will be told to keep the leg straight for a few hours after the procedure to minimize the chance of bleeding at the catheterization site.
Surgical repair (PDA surgery) : - Some children who undergo PDA ligation may need to spend some time in the intensive care unit after surgery. Others may return to a regular hospital room. Your child will be kept as comfortable as possible with medications which relieve pain or anxiety. The staff will also be asking for your input as to how best to soothe and comfort your child.
 Pulmonary valve stenosis Pulmonary valve stenosis
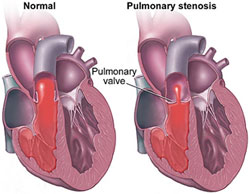
Pulmonary valve stenosis is a condition in which the flow of blood from the heart (right ventricle, or lower chamber) is blocked at the valve that separates the heart from the pulmonary artery (pulmonic valve). This narrowing is usually present at birth (congenital).
Causes
Pulmonary valve stenosis is most often caused by a problem that occurs when the unborn baby (fetus) is developing. The cause is unknown, but genetics may play a role. Narrowing that occurs in the pulmonary valve is called pulmonary valve stenosis. Narrowing that occurs below the pulmonary valve is called subvalvar pulmonary
stenosis. Another form of the condition, supravalvar pulmonary stenosis, is when narrowing occurs above the main pulmonary valve.
The defect may occur alone. However, it can also occur with other heart defects. The condition can be mild or severe. It occurs rarely, in only about 10% of patients with congenital heart disease.
Pulmonary stenosis can also occur later in life as a result of conditions that cause damage or scarring of the heart valves. These include rheumatic fever, endocarditis, and other disorders.
Symptoms
Bluish coloration to the skin (cyanosis) in some patients, Chest pain, Fainting, Fatigue, Poor weight gain or failure to thrive in infants with severe, blockage, Shortness of breath
Note: Patients with mild to moderate blockage may not have any symptoms. There may be no symptoms until the disorder is severe. Symptoms, when present, may get worse with exercise or activity.
Diagnosis
The health care provider may hear a heart murmur by stethoscope. Tests used in the diagnosis of pulmonary stenosis may include:
- Cardiac catheterization
- Chest x-ray
- ECG
- Echocardiogram
- MRI of the heart
Treatment
Sometimes, treatment may not be required.Percutaneous balloon pulmonary dilation (valvuloplasty) using a catheter can be successful for pulmonary valve stenosis that occurs without other heart defects. Surgery may be performed to repair the defect. Medications used before surgery may include:
- Anti-arrhythmics to improve the heart function
- Blood thinners to prevent clots
- Prostaglandins
- Water pills to remove the excess fluid
Outlook (Prognosis)
As a general rule with mild stenosis, one-third of patients get better, one-third stay the same, and one-third get worse. The outcome is good with successful surgery or cardiac catheterization. Other congenital heart defects may also be a factor.
Possible Complications
- Cyanosis
- Death
- Heart failure
- Leaking of blood back into the right ventricle (pulmonary regurgitation) after repair
- Right ventricular hypertrophy (enlargement)
|