| Faqs |
|
For the convenience of our visitors
we have categorized the Frequently Asked Questions.
Kindly click on the elated category below to view
the FAQs on that particular subject.
- Digital X-Ray
- Full Length X-ray
- 2D Echo - Two Dimensional
Echocardiography
- Bone Densitometry
- Whole Body True Fan Beam DXA Bone Densitometry
- Color Doppler
- Computerized Pathology
- CT Scan Or CAT Scan
-Spiral Computed Tomography
- Cardiac CT
- Mammography
- MRI - High Strength
Magnetic Resonance Imaging
- Sonography Or Ultrasound
- Stress Test
- X-rays Diagnostics
Radiology
- Other Radiology
Procedures (IVU/IVP, MCU, DRU, Sialography, fistulography,
sinusography, orthography)
- OPG
- Nutrition &
Diet
|
| Digital
X-Rays - Plain Films |
What are X-rays?
X-rays are electro-magnetic radiation, which are produced
by special machines called X-ray machines. These cannot
be seen, felt or heard.
How do X-rays work?
Different parts of the body behave differently with
X-rays. Structures such as bone absorb X-rays, whereas
air in the lungs lets all X-rays pass through. Thus,
when X-rays pass through the body, when they come
out, they have different strengths, depending on what
parts of the body they have passed through. When these
X-rays hit a film (like a photographic film), that
film gets exposed depending upon this variation. Like
a photographic film, this special film also needs
to be developed, before we can see the final picture.
Where are X-rays useful?
X-rays have been used to look at all parts of the
body. Specifically, they are required for the chest,
all bones and joints and for the abdomen.
Are there any dangers?
Since, X-rays involve radiation, there is a theoretical
risk, though none in practice. In women who are pregnant,
X-rays should be performed only after weighing all
risks and benefits.
What are the dyes used with X-rays?
Sometimes, artifical dyes are used to improve our
ability to see internal structures. These usually
form part of a "procedure". The common dyes
used are either barium containing (barium sulphate)
or iodine containing. Barium sulphate is used for
all barium examinations to study the stomach and intestines.
Iodine containing dyes are usually injected in the
veins to study the kidneys, during mammography, etc.
Are there any complications of the dye?
Five % of patients may get nausea and redness of skin.
Though severe reactions are known, these are very
rare and uncommon. However, in patients having
a previous history of allergy, those who are asthmatics,
those with renal and cardiac failure, a special dye
which is more expensive, but safer should be used,
to prevent a reaction.
Who is qualified to report X-rays?
Only radiologists are trained to read X-rays and all
X-rays should carry a radiologist's report. Other
physicians and non-radiology centres may also perform
X-rays, but they are usually not qualified. Before
going for an X-ray, ask the centre, whether it will
be done under the radiologist's supervision.
Are there any newer advances in X-rays?
X-rays are used in CT scanning (computed tomography).
Digital radiography uses X-rays for directly producing
images on a computer, bypassing the film - this is
very helpful in emergency situations, such as the
trauma centre or intensive care unit.
What are Digital X-rays?
All images obtained
using digital systems are digital x-rays. The commonest
digital method used is the CR system that produces
digital X-rays on a computer. See the accompanying
picture for an idea of how this works.
What are the advantages of Digital X-rays
Digital X-rays are superior to conventional
X-rays in resolution and quality.
Top
|
| Full
Length Digital X-Rays |
What are Full Length Digital
X-rays?
Full-length radiographs are important radiographs
in orthopedics, where x-rays of the whole spine or
the entire lower limbs are obtained. These are mainly
indicated for measurements of length and angles and
important prior to some types of surgeries.
Why are Full Length X-rays such a big deal?
Traditionally, it has been difficult to obtain full-length
radiographs in our part of the world on a regular
basis - many of us have tried local, ingenious methods
of getting those three or two radiographs and taping
them together.With the digital x-ray technology, we
are now able to "stitch" multiple radiographs
to obtain full-length images, which are then printed
on one film. Two representative examples are given
alongside. |
  |

Top
|
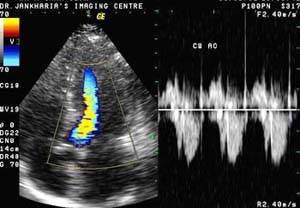
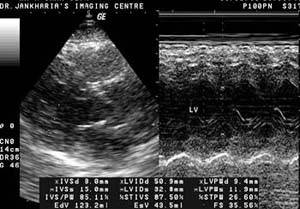
2D
Echo – Two Dimensional Echocardiography |
 |
 |
Q1. How is it performed?
A. The echocardiogram will be performed
and recorded by a specially trained cardiologist.
It usually takes approximately one-half hour. Since
the transducer must be placed directly on the chest
wall or upper abdomen, you will be asked to disrobe
from the waist up.
You'll be asked to lie down and small adhesive patches
will be attached to your body to record your electrocardiogram.
The electrocardiogram is useful for timing of the
heart cycle. Your physician may request that an echocardiogram
be performed simultaneously with an exercise test.
This procedure will be thoroughly explained by the
physician or Cardiologist.
At times during the test you may be asked to hold
your breath, change position or refrain from talking
in order to get a better picture. The Cardiologist
will tell you if this is necessary.
Q2. Is it dangerous?
A. Ultrasound cannot be felt and
does not hurt. There are no known harmful or proven
side effects from ultrasound. If you are pregnant
during the time an echocardiogram is performed there
is no known danger to either mother or baby from this
procedure.
Q3. What are the procedures involved that
one should know about beforehand?
A. To improve the quality of the
picture, a harmless, odorless and water-soluble gel
is applied to the area of your skin where the transducer
will be placed. This may feel cool and a bit moist,
but the gel will be wiped off thoroughly after the
examination.
During the procedure you might feel a slight pressure
and/or vibrations from the transducer. This should
not be painful. Tell the Cardiologist if you become
uncomfortable. The room lights will be dimmed to reduce
any glare and to better see the monitor.
Q4. What happens after the procedure?
A. Although the Cardiologist who
is performing this test may explain what is being
seen on the screen as the examination is in progress,
it is essential to obtain precise measurements from
the paper and videotape recordings. If you have had
previous echocardiograms, the new ones will be compared
with those and the cardiologist will analyze any differences.
Your doctor will review with you the results and
final diagnosis.
Top |
Bone
Densitometry |
Q1. What is
Bone Densitometry?
A. Bone Densitometry (BMD) is currently accepted
as being a quick, simple, painless examination that
is currently the most sensitive screening tool used
to detect bone loss in early stages of osteoporosis.
It also is the least expensive and most cost effective
method for this type of examination.
Q2. Is there any radiation involved?
A. BMD uses an extremely small amount of
X-rays (less than 1/10 that used for a chest X-ray)
to measure the thickness or density of your bones.
The exam takes less than 15 minutes.
Q3. How does it work?
A. Bone Densitometry is a tool used to predict
the possibility of a fracture. The resulting measurements
of your bone density are compared to what is expected
of someone your age, sex, size and ethnic background.
It is also compared to what is estimated to be bone
density of a young healthy adult of the same sex.
The information allows your doctor to determine if
you have osteoporosis and the likelihood of a fracture
happening. The best course of treatment can then be
determined.
The ability of BMD to predict fractures is undisputed.
It is similar to blood pressure predicting strokes
and is more effective than using cholesterol to predict
heart disease.
What is the procedure involved in the examination?
A DXA scan involves laying on a couch for approximately
10 minutes while a tiny X-ray detector scans your
spine, your hip or both. The scan itself is safe and
painless.
Q4. Who is at Risk?
A. In India, 1 in 6 women over 50 years old
will break their femur (hip), while 1 in 4 will suffer
severe fractures in one or more bones.
The death rate from osteoporosis-related fractures
is greater than deaths caused by breast and ovarian
cancer combined!
Some authorities believe you may be at risk for osteoporosis
if you have one or more of the following:
- Family history of osteoporosis
- Early menopause either natural or surgical
- Amenorrhea (lack of periods) particularly in young
woman
- Anti-seizure medicine for many years
- Hyperthyroidism or hyperparathyroidism
- Cushing's syndrome
- Kidney failure colitis
- Stomach or intestinal surgery
- High intake of alcohol, coffee, tea or soft drinks
- Heavy smoking
- Low dietary intake of calcium
- European or Asian ancestry
Top |
Color
Doppler |
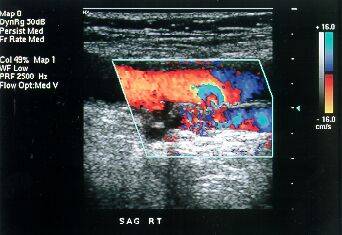
Q1. What is Color Doppler?
A. Color Doppler is a special ultrasound
technique, which allows us to evaluate blood vessels.
Q2. What is the principle?
A. Using the Doppler principle of changing
pitch with velocity, ultrasound waves that reflect
from the red blood corpuscles in arteries and veins
are evaluated for velocity and amplitude and color
maps of the vessels can be generated.
Is special equipment required?
An ultrasound machine equipped with color Doppler
facilities is required. These are now readily available
at many centers.
Q3. What is its utility?
A. Color Doppler is very useful in evaluating
the carotid arteries in the neck, the heart (echocardiography),
the arteries and veins in the abdomen and the arteries
and veins in the upper and lower limbs.
Q4. What is power Doppler?
A. It is a type of color Doppler.
Q5. Is any special preparation required?
A. No
Q6. What is the cost?
A. The cost varies from type to type depending
on the kind of Colour Doppler being done.
Q7. Who is qualified to perform color Doppler?
A. A qualified radiologist is the only one
who should perform color Doppler examinations.
However, Cardiac Color Dopplers are performed by
qualified cardiologists.
Q8. What are the contraindications in Color
Doppler?
A. There are no contraindications for color
Doppler but like all other forms of cardiac ultrasound,
technically poor studies may be obtained in patients
with chronic lung disease or obesity. Additionally,
the registration of color Doppler decreases in the
far field and flow abnormalities may not be obvious
in areas distant to the transducer.
Top |
Computerised
Pathology |
Q1. Is Fasting required for
routine investigations?
A. Yes fasting is required for most of the
routine hematology and biochemical investigations
unless specified otherwise by the doctor.
Q2. When can I get the report?
A. 90% of reports can be given on the same
day evening and certain specialized investigations
can be done in a day or two.
Q3. Do you use disposable collection device?
A. Yes, for every patient fresh blood collection
device is used which is then disposed with due precautions.
Q4. Do you offer home visit for blood collection?
A. Yes, with prior notice, we send technicians
for home visits within vicinity of our centres.
Top |
CT
Scan |
Q1. Is it uncomfortable? Is
it dangerous?
A. The test itself is completely painless.
You will be asked to lie quietly on the CT scanner's
"patient couch" during the study. Depending
on the type of study being done, you may be injected
with, or be asked to drink, contrast material.
Because contrast agents contain iodine, which causes
an allergic reaction in some individuals, be sure
to tell the technologist, nurse or radiologist if
you have had an allergic reaction to these agents
before, or if you have any other allergies.
CT scanners use x-rays. For your safety, the amount
of radiation is kept to an absolute minimum and our
equipment is kept in top shape. Because x-rays can
harm a developing foetus, however, be sure to tell
your doctor if you are, or think you may be, pregnant
before preparing for the CT exam. Even if you haven't
told your doctor, be certain to tell the CT scan technologist
who prepares you for the study.
Q2. How is a CT Scan done?
A. The technologist will bring you into the
CT scan room where you will lie down on the patient
couch (usually on your back). You should get comfortable
because it is very important that you not move during
the test. CT examinations differ depending on your
medical problem and the part of your body being studied.
The radiologist will plan an examination that is best
suited for you.
For example, if your abdomen is being studied, a series
of pictures will be taken from your lower chest down
to the upper pelvis. During such a study, you will
be asked to hold your breath so that the pictures
will not be blurred. The machine will make some noise,
and the couch may move slightly after each picture.
Also, you may receive signals from the technologists
(or from the machine) about your breathing. As part
of your test, before or during the study, you may
be given an injection (by a nurse, technologist or
doctor) of a contrast agent. This allows the radiologist
to obtain clearer images of your organs. Should you
have any discomfort during the test or after the injection,
tell the technologist. All the CT personnel are trained
and certified and know how to help you.
Q3. What happens after the scan?
A. Once the CT staffs are sure that enough
information has been collected, you may leave and
go about your normal activities without restriction.
Q4. When do I get the results?
A.Our radiologists who specialize in this
type of imaging will review your exam. Reports will
be made available online.
Q5. What the patient should tell the doctor:
A. The patient should volunteer information
to the radiologist if he has ailments like asthma,
heart or kidney disorders, history of allergy, diabetes,
or a previous reaction to contrast media. It is most
important for the radiologist to have this information
so that he can choose a contrast medium most suitable
to the patient.
Q6. What if I have other questions?
A. If you have any questions about your CT
scan, please ask any of our personnel (physicians,
nurses, technologists, receptionists). We will try
our best to explain the procedure clearly and to make
your visit to the CT suite as comfortable and speedy
as possible.
Top |
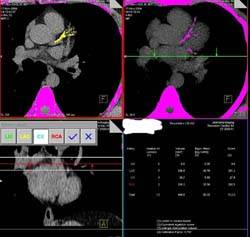
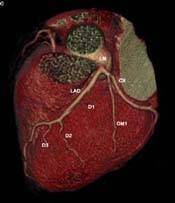
Cardiac
CT |
Why is it
called Ultra-Fast CT?
A regular CT has tube rotation speed of 1 or .75 seconds.
This CT has tube rotation speed of 330ms, i.e. approximately
3 rotations per second. This allows extremely fast
scans of the body, such that routine chest and abdomen
sequences can be completed in 3-5 seconds. That is
why it is called Ultra-Fast CT.
How does cardiac CT work?
With such a fast scanner, it is possible to "freeze"
the heart. The new 64-slice scanner obtains almost
194 slices per second. After gating with the ECG,
it is possible to scan the heart in 10-12 seconds
and to extract information about the coronary arteries
and cardiac function from the dataset.
What preparation is involved?
4 hours fasting before the procedure
Stabilization of heart rate with a beta-blocker
Getting all old cardiac related information.
What does the procedure involve?
Once the heart rate is stabilized
A vein is cannulatedo Breathing instructions are given
so that the patient can hold his/her breath for around
12 seconds
A calcium scoring study is performed
The "dye" is injected and the angiogram
study is performed
The angiogram time is 10-12 seconds. The entire procedure
takes between 15-60 minutes depending on the heart
rate.
What are the various parts of the study?
The following 3 parameters are studied
- Calcium scoring
- Coronary artery assessment
- Functional assessment (wall motion and ejection
fraction)
What are the indications?
Patients at high risk for developing coronary artery
disease (high triglycerides, family history, smoking)
Follow-up of known mild to moderate untreated disease
Post-bypass assessment
Are there any dangers of CT scanning?
Though X-rays involve radiation, there are no dangers,
in practice. In women who are pregnant, however, CT
scanning should be done after weighing all the risks
and benefits.
What is the injection
that I will receive?
The majority of patients will be injected with a "dye"
which enhances the ability of CT scans to pick up
abnormalities. This is routine. Only a non-ionic dye
(the safest) is used.
Are there any complications of the "DYE"?
0.5% of patients may get nausea and redness of the
skin. Though severe reactions are known, these are
very rare and uncommon. |
Are there other instructions?
Please get all old X-rays, Sonography, CT and MR films
along with other papers, operative notes, discharge
cards, etc. relevant to the case. Please come fasting
for at least six hours, prior to the scan. There should,
preferably be an accompanying friend or relative.
Please inform the doctor, nurse
or the receptionist, if you are at high risk for "dye"
injection, as described above, i.e. if you have a
history of drug reactions, bronchial asthma, cardiac
or kidney disease, etc.
Please inform the doctor, nurse or the receptionist
if you are pregnant or think you may be pregnant.
Top |
Mammography |
Q1. What is
mammography?
A. Mammography is x-rays of the breasts so
as to enable one to detect early breast cancer.
How is it performed?
It is similar to taking X-rays of the chest or any
other X-rays. However, a special dedicated machine
with a special X-ray tube is required for doing mammography.
There are compression paddles which compress the breast
and then X-rays are taken. Usually, two views of each
breast are performed, with a total of four X-ray films
per patient.
Why should it be done?
Mammography is performed for screening for breast
cancer. Also, in patients with lumps in the breast,
mammography helps in the diagnosis of the lump, i.e.
whether it is benign or malignant. In simple words,
it helps to know whether it is cancer or not.
If I have no complaints relating to the breast, should
mammography be done?
Yes. The most important role of mammography is for
screening normal women for early breast cancer. Breast
cancer can be picked up by mammography much before
it develops into a palpable lump.
How does it do that?
There are early signs of breast cancer like microcalcifications
and small densities which can be seen on mammography
much earlier than when it forms a mass which can be
felt.
When should mammography be performed?
The American Cancer Society suggests that between
40 - 49 years, mammography should be performed every
1-2 years. At and over 50 years of age, mammography
should be performed yearly.
Is there any preparation required for mammography?
No. You can just do it at any time. No preparation
or fasting is required. Please do not use any powders
or deodorants on the breasts or arm-pits prior to
this procedure as these give rise to artefacts on
X-Rays.
Who will be doing it on me?
Only trained women personnel will be performing it.
Not only will they be understanding and compassionate
while performing it, but also they can counsel you
on regular Breast Self-Examination if you have not
understood it with the other pamphlets provided.
Who will be interpreting these mammograms?
The interpretation will be done by qualified radiologists
with specialised training in mammography. Also, the
doctor will be available for any queries on the subject
and please do not hesitate to clear any doubts that
you may have.
Q2. Does mammography itself cause breast cancer
because of radiation?
A. The radiation exposure with mammography
is very less. Also if the pros and cons of mammography
are weighed, the pros outweigh the cons by far. The
radiation effect on the breasts decreases exponentially
after 35 years of age. The only precaution to be taken
is that the patient should be sure that she is not
pregnant.
Q3. Does the procedure of mammography cause
pain?
A. With newer equipment very little discomfort
is felt by the patient. The patient should preferably
come after the period is over, as the likelihood of
pain will be the least. However there will be no changes
in the findings on mammography during any stage of
the menstrual cycle.
Q4. What is sonomammography? Why do mammography
when everything is seen on sonomammography?
A. Sonomammography is sonography of the breasts.
It is usually done as a complementary procedure to
mammography. It helps in distinguishing a cystic mass
from a solid mass. Cysts are usually benign. Mammography
is required as the earliest of cancers are seen only
on this modality.
Q5. Can one definitely tell whether a mass
is benign or malignant?
A. It is not possible to tell 100% whether
a mass is benign or malignant on either mammography
or sonography. To be 100% sure, a biopsy is required.
Sonography and mammography, both together are 95%
accurate in diagnosing a lesion.
Q6. If a close relative has breast cancer,
what are the chances of a person getting it?
A. The chances are 5-15% if it is a first
degree relative particularly on the maternal side.
The person is at a high risk & should start doing
mammography 10-15 years earlier than the age at which
the relative got breast cancer.
Q7. How does breast cancer usually present
itself?
A. Breast cancer usually presents itself
as a lump. Therefore a patient should regularly do
a monthly self-breast examination particularly after
the period is over. Sometimes there might be a bloody
nipple discharge. Occasionally in 10% of the patients,
there is associated pain.
Does breast cancer occur in men also?
Yes. 1% of all breast cancers do occur in males. But
since the incidence is quite low, they need not do
screening mammography. However, if a lump occurs in
the breast region of a man, mammography can be performed.
What is Breast Self-Examination?
Breast Self-Examination or BSE is palpation of the
breast by women with their own fingers to look-out
for lumps.
Top
|
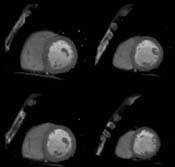
MRI |
Q1. What is
an MRI scan?
A. "MRI," which stands for "Magnetic
Resonance Imaging," uses a powerful magnet
and precisely programmed radio signals to "see"
inside the body, beyond what an x-ray can see. MRI
shows normal anatomic structures (brain, organs, blood
vessels, etc.) as well as structural or chemical alteration
of tissue by disease. With MRI, it is often possible
to diagnose disease at a very early stage, before
it is visible by other means. Because most diseases
are better treated when found early, MRI scans are
becoming increasingly useful.
Q2. Is it uncomfortable? Is it dangerous?
A. MRI is completely painless and safe for
most people. However, MRI cannot be performed in a
few cases on certain individuals, such as those who
have cardiac pacemakers or certain other metal implants.
If you have had any surgical implants, please discuss
this with your doctor. With technological advances
though, today most surgical implants are MRI compatible
so one need not worry about the same.
Q3. How long does it take?
A. An MRI scan typically takes from 30 to
60 minutes to complete. However the time differs depending
on the type of MRI being done.
Q4. What happens on the day of the scan?
A. Plan to arrive at the MRI suite at least
15 minutes before your scheduled appointment. This
will allow time to prepare the necessary paperwork.
You will be asked to fill out a brief questionnaire
about your medical history, medications, and allergies.
An MRI technologist will introduce herself/himself
to you, explain the test you have having, and answer
your questions. You will be asked to change into a
gown and to remove any metal objects (belt buckle,
watch).
Q5. What happens during the scan?
A. In the MRI suite you will be asked to
lie on a narrow, movable table that will gradually
slide you through the circular bore of a large, doughnut-shaped
magnet. You should get comfortable because it is very
important that you not move during the scan.
MRI procedures differ depending on your medical problem
and the part of your body being studied. The radiologist
plans an examination that is best suited for you.
For example, if we are studying your abdomen, we will
examine from your lower chest down to the upper pelvis,
producing several series of images. During such a
study, expect the machine to make loud noises, the
tables to move occasionally, and the technologist
to instruct you about your breathing.
In some cases, in order to enhance the MRI images
and to visualize diseased tissues, the doctor will
request the injection of an MR contrast agent, which
is injected intravenously. Side effects are rare.
Anyone who has had recent surgery with surgical staples
needs to be able to communicate with the technologists
to tell us if there are any burning sensations. Anyone
with a reprogrammable shunt must have the shunt reprogrammed
after the MRI. And anyone with the possibility of
having metal in their eyes (for example, one who does
metal work as a career may have tiny bits of metal
in the eyes that can be affected by the MRI), should
have an ORBITS (x-ray of the eye) to rule out foreign
bodies.
Remember, each examination is tailored to individual
requirements. Additional pictures are usually taken
after the first series is completed.
Q6. What happens after the scan?
A. Once enough information has been collected,
you can leave and go about your normal activities
without restriction.
Q7. How do I get the results?
A. Radiologists who specialize in this type
of imaging will review your exam. You will then be
asked to collect your report online.
Q8. Any questions?
A. If you have any questions about your MRI
scan, please ask any of our personnel including doctors,
nurses, or technologists. We will try our best to
explain the procedure clearly and to make your visit
to the MRI suite as comfortable and speedy as possible.
Top |
Sonography |
Q1. What is sonography?
A. Sonography, or ultrasound, utilizes high
frequency sound waves (not x-rays) to obtain diagnostic
images. Ultrasound imaging is used to evaluate many
parts of the body, including the abdomen, blood vessels,
fetus of pregnant women, superficial body structures,
and newborn brain to name only a few.
Q2. What is the importance of sonography today?
A. Ultrasonography enables to detect and
investigate:
- All diseases of the organs of the abdominal cavity
in early stages
- Tumors of uterus and ovaries and abnormalities
of reproductive organs
- Maturation of eggs and changes of endometrium
in different stages of menstrual cycle
- Early pregnancy, including ectopic pregnancy
- Development of fetuses and possible malformations
of fetuses
- Position of the fetus, position of the placenta
in the uterus and changes in it. It is also possible
to estimate the quantity of -amniotic fluid, evaluate
heart
- Function and breathing movements of the fetus.
Q3. What are the limitations
of sonography?
A. Ultrasound waves cannot penetrate air
& bone and hence sonography has limited applications
in regions like the skull and chest
Q4. Is sonography harmful?
A. No harmful effects of sonography are known
even on the embryo of the foetus of a pregnant women..
Q5. What is Colour Doppler?
A. Colour Doppler is colour-encoded sonography
of the blood vessels. Blood flow is seen in colour.
It is like sonography and there is no involvement
of any injection of contrast
Q6. What is 3D sonography?
A. 3D sonography is 3 Dimensional display
of the surface of a structure like a foetal face/spine
or any other part of the body.
Q7. What is endovaginal sonography?
A. It is sonography done for better visualisation
of uterus & ovaries. A high-resolution endovaginal
probe is inserted into the vagina for this examination.
It is not painful.
It is done as a routine at our centre as it is observed
that at times even fairly prominent lesions can be
missed if only trans-abdominal sonography is performed.
It does not require a full bladder.
Q8. Is dating and weight estimation 100% accurate?
A. Dating and weight estimation are just
estimates based on statistical data of the baby size.
It is not 100% accurate but predicts the dating and
weight estimation up to +/- 10%.
Top
|
Stress
Test |
Q1. How is the test carried
out?
A. A stress test or treadmill test or exercise
records the hearts electrical activity (rate and rhythm)
during exercise.
- Prior to the test electrodes will be placed on
the chest (same as ECG) and patient is hooked up
to equipment to monitor the heart.
- Prior to the test you may be asked to breath
rapidly (hyperventilate) for a while.
- The patient will be asked to walk on a monorised
treadmill.
- The speed and inclination of the treadmill will
be gradually increased.
- The doctor will be looking for changes in ECG
pattern, will check Blood Pressure in between and
will be enquiring about any symptoms that the patient
may experience.
- The patient may be on treadmill for up to 15
minutes, depending upon his level of exercise recovery
and cardiovascular -condiovascular conditioning.
- The test will be stopped if the patient becomes
too tired, has any symptoms such as chest pain.
Q2. What happens after the
test is done?
A. After the test patient will be
asked to sit or lie down till heart and blood pressure
recovers to baseline. The stress test doctor will
then evaluate the data collected through the test
and make the necessary recommendations.
Q3. How long does a normal stress test take?
A. The total time required for the
test will be about 30 minutes.
Q4. Is there any risk in taking the test?
A. There is very little risk in taking the
test in healthy person - no more than if a person
walks fast or jogs up a big hill.
During the test the cardiologist and a technician
are always present.
Q5. Why is a stress test done?
To find out:
How hard the heart can work before symptoms develop.
How quickly the heart recovers after exercise.
The patients overall level of cardiovascular conditioning
Q6. Is it necessary to take a prior appointment?
A. Prior appointment will save considerable
time on the day of test.
Top |
Diagnostic
Radiology |
Q1. How significant is the
radiation in an X-ray?
A. The average amount of exposure to an X-ray
is very low and is well within the acceptable amount
recommended.
Q2. What does one do if an X-ray is required
during pregnancy?
A. The X-ray technician should be informed
and he should cover the lower abdomen with a lead
apron. In case one's pregnancy status is unknown,
it is still a good idea to ask for protective cover.
What are barium studies?
These are studies of the gastro-intestinal performed
using barium sulphate and x-rays.
Why are there different types of barium studies?
Depending on the area being examined, we have barium
swallow, meal, meal-follow-through, enema and small
bowel enema.
What are these?
Barium swallow is a study for the esophagus, barium
meal for the stomach, barium meal follow-through for
the small bowel, barium enema for the large bowel
and small bowel enema for the small bowel. In swallow,
meal and meal-follow-through examinations, the patient
has to drink barium. In barium enema examinations,
barium is injected using an enema tube. In small bowel
enema examinations (enteroclysis), a tube is inserted
from the nose to the duodenum and barium is injected.
How do barium examinations work?
Barium is an inert substance that coats the internal
lining of the bowel and fills up its lumen. It is
radio-opaque and thus seen very well on x-rays.
Is there any danger?
Barium by itself is an inert substance and completely
harmless. However if it escapes into the abdominal
or thoracic cavity through a perforation, it can cause
severe inflammation. Thus barium studies should not
be done in patients with suspected perforation.
What preparation is required?
For barium swallow, none. For barium meal, at least
six hours fasting. For barium meal follow-through,
overnight fasting with Dulcolax tablets for clearing
the bowel. For small bowel and barium enema, overnight
fasting with liquid diet the day before and aggressive
clearing of the bowel with Dulcolax tablets the night
before and in the morning.
Q3. Isn't barium awful to taste?
A. No it is pleasantly flavoured.
Q4. How long does a barium test take to perform?
A. An upper G.I. series takes 30 minutes.
A full study takes 3-4 hours.
Q5. In these days of hi-tech investigations,
are X-rays getting redundant?
A. No, X-rays are a very cost effective means
of diagnosis, particularly where diseases of chest,
bones & joints are concerned.
Top
|
Other
Radiology Procedures (IVU/IVP, MCU, DRU, sialography,
fistulography, sinusography, arthrography) |

IVU (intravenous urography)
In this, a dye is injected intravenously and x-ray
pictures of the kidneys, ureters and bladder are obtained.
The dye is radio-opaque and seen well with x-rays.
Overnight fasting and good preparation of the colon
with Dulcolax are required.
MCU (micturating cystourethrography)
Dye is introduced into the urinary bladder and the
patient is asked to micturate/urinate. X-ray pictures
are obtained during the act of micturition to assess
the function and structure of the urinary bladder
and urethra.
RGU (retrograde urethrography)
Dye is injected through the urethra from the glans
penis and x-ray pictures are taken. This helps in
assessing the urethra and the bladder base.
Fistulogram and sinusogram
In these studies, using a small catheter, iodinated
dye is injected into the cutaneous sinus or fistula
and x-rays are taken, which help in identifying the
tract of the sinus or fistula.
Sialography
In this, the parotid duct is cannulated from the mouth
and x-ray pictures of the parotid duct and gland are
obtained.
Angiography, venography
The arteries are catheterized usually through the
femoral artery and after injection of iodinated dye,
x-rays are taken. If the same study is performed for
the veins, we get venograms.
HSG (hysterosalpingography)
The cervix is cannulated and iodinated dye is injected
into the cervical and uterine lumen. The Fallopian
tubes are then well seen. This procedure is used to
study the patency of the passage as well as other
structural abnormalities.
Top
|
OPG
(Orthopantomogram) and Cephalogram |

What is OPG?
OPG stands for Orthopantomography. It is a special
method for obtaining radiographs of the teeth-bearing
jaws, both upper and lower.
How is it different from regular X-ray machines?
A regular X-ray machine cannot take detailed pictures
of the jaw-bones. An OPG machine is specially constructed
so that it rotates around the jaw-bones, thus giving
us an extremely good idea about the structure of the
jaw bones. Yes, x-rays are used, but the method is
totally different.
In what situations are they needed?
OPG x-rays are usually asked for by dentists, whether
they be general dentists, orthodontists, oral surgeons
or prosthodontists/implantologists. Because OPGs give
a bird-eye view of the teeth and the adjacent bones,
they are useful in a wide-variety of conditions including
infections, tumors, congenital abnormalities, pre-implant
evaluation and trauma.
Are they any risks?
Just as with x-rays elsewhere in the body, if a lady
thinks she might be pregnant, an OPG can be avoided.
No other risks exist.
Is any dye injected?
No
How much time does it take
to get OPGs done?
Around 10 minutes.
Top |
Nutrition
& Diet Food |
- Fat content in various common foods
- Calorific values of some indian/continental/fast
foods
- High protein foods
- Dietary sources rich in calcium
- Foods high in cholesterol
- Foods to avoid for gout trouble (high uric
acid levels)
Fat content in various common foods
| FOODS
|
QUANTITY
|
FAT (gms)
|
Diary products
|
Buffalo milk |
85 ml |
7.5 |
Cow’s milk |
150 ml |
6.0 |
Curds |
170 gms |
7.0 |
Cheese |
30 gms |
7.0 |
Whole milk powder |
20 gms |
5.3 |
Skimmed milk liquid |
350 ml |
3.0 |
Egg yolk |
1 in no |
6.7 |
Egg white |
1 in no |
Nil |
Skimmed milk powder |
30 gms |
Nil |
Paneer (cow’s
milk) |
40 gms |
8 gms |
Paneer (buffalo
milk) |
40 gms |
8 gms |
Pulses |
30 gms |
0.5 gms |
Cereals |
28-31gms |
0.5gms |
Soya bean |
20 gms |
4.4 gms |
Soya milk |
200 ml |
1 gm |
Meat products
|
Beef |
90 gms |
2 gms |
Pork |
90 gms |
4 gms |
Mutton |
50 gms |
7.0 gms |
Liver |
90 gms |
3.0 gms |
Chicken |
90gms |
0.5 gms |
Lean meat |
90 gms |
3.0 gms |
Sea Food |
Fish (dry) |
35 gms |
2.0 gms |
Fish (fresh) |
100 gms |
20. gms |
Crab |
170 gms |
20. gms |
Nuts |
Almonds |
100 gms |
32 gms |
Cashewnuts |
100 gms |
32 gms |
Walnuts |
100 gms |
64 gms |
Peanuts |
100 gms |
72 gms |
Coconut(fresh) |
23 gms |
9.5 gms |
Calorific values of some Indian / Continental
/Fast foods
| FOODS
|
QUANTITY
|
ENERGY
(K cals) |
Egg boiled |
1 in no |
85 |
Egg poached |
1 in no |
85 |
Egg fried |
1 in no |
110 |
Egg omelette |
1 in no |
175 |
Puri |
1 in no |
150 |
Dosa (masala)
|
1 in no |
250 |
Cooked rice(plain)
|
100 gms |
120 |
Nan |
1 in no |
150 |
Curry meat |
1 cup |
175 |
Salads |
100 gms |
50 |
Pickle |
5 gms |
30 |
Coffee,black (w/o)
sugar |
1 cup |
10 |
Tea with milk
and sugar |
1 cup |
45 |
Fruit juices |
1cup |
120 |
Soft drinks |
1 bottle |
90 |
Ice-cream |
1 cup |
200 |
Butter |
1 tea spoon |
35 |
Ghee |
1 tea spoon |
45 |
Fried nuts |
1 cup |
300 |
Mayonnaise |
1 tea spoon |
45 |
Margarine |
1 tea spoon |
45 |
Bread slice with
butter/jam/cheese |
1 in no |
150 |
Break Fast cereals
with milk |
1 bowl |
100 |
Baked beans in
sauce |
1 cup |
200 |
Sausage/bacon/ham
|
1 helping |
120 |
Potato 9fried)
|
1 cup |
200 |
Sandwich(large)
|
1 piece |
250 |
Hamburger |
1 piece |
250 |
Steak and salad
|
1 plate |
300 |
Fish and chips
|
1 plate |
400 |
Sphaggetti and
meat sauce |
1 plate |
450 |
Baked dish |
1 helping |
450 |
Chineese noodles
|
1 plate |
450 |
Pizza |
1 plate |
400 |
High Protein
Foods
| FOODS
|
QUANTITY
|
PROTEIN
|
Pulses |
30 gms |
7.0 gms |
Soyabean |
20 gms |
10.0 gms |
Soya milk |
200 ml |
40. gms |
Green peas |
100 gms |
8.0 gms |
Lean meat |
90 gms |
18.0 gms |
Liver |
90 gms |
19.0 gms |
Chicken |
90 gms |
24.0 gms |
Egg white |
1 in no |
3.5 gms |
Cow’s milk
|
150 ml |
5.0 gms |
Cheese |
30 gms |
7.0 gms |
Skiimed milk powder
|
30 gms |
11.0 gms |
Skimmed milk liquid
|
350 ml |
9.0 gms |
Curds |
170 gms |
50. gms |
Panner (cow’s
milk) |
40 gms |
7.0 gms |
Paneer (buffalo’s
milk) |
35 gms |
4.5 gms |
Crab |
170 gm |
15.0 gms |
Fish(dry) |
35 gms |
20.0 gms |
Fish (fresh) |
100 gms |
20 gms |
Dietary sources rich in calcium
| FOOD ITEMS
|
CALCIUM
(Milligram per 100 gram) |
Meat Products
|
Chicken/ meat
|
30 |
Mutton (muscle)
|
150 |
Pork(muscle) |
30 |
Crab(muscle) |
1370 |
Prawn |
320 |
Mackerel (bangada)
|
430 |
Rohu |
650 |
Egg (hens) |
60 |
Nuts |
Almonds |
230 |
Ground nuts |
50 |
Pistachio |
140 |
Dairy Products
|
Milk(cow’s)
|
120 |
Milk(buffalo’s)
|
210 |
Curds (cow’s
milk) |
120 |
Cheese |
790 |
Skimmed milk powder
|
1370 |
Milk powder whole
|
910 |
Vegetable
and fruits |
Cauliflower |
140 |
Fenugreek |
470 |
Spinach |
60 |
Lady’s finger
|
90 |
Beet root |
200 |
Cabbage |
80 |
Figs |
60 |
Grapes (blue)
|
30 |
Dates |
70 |
Oranges |
50 |
Raisins |
100 |
Apple |
10 |
Banana |
10 |
Papaya |
10 |
Cereals &
Pulses |
Bajra |
50 |
Ragi |
30 |
Whole wheat flour
|
50 |
Refined wheat
flour |
20 |
Rice(raw/par boiled)
|
10 |
Rice (flakes/puffed)
|
20 |
Soya bean |
240 |
Dal |
160 |
Black gram dal(udad)
|
200 |
Foods high in Cholesterol
- Red Meat
- Egg Yolk
- Mutton
- Liver
- Pork
- Lamb
|
- Butter
- Whole Milk
- Ghee
- Margarine
- Mayonnaise
- Oil
- Cream
|
- Nuts
- Dry Fruits
- Ice-Creams
|
Foods to avoid for gout trouble (high uric
acid levels)
- Organ meats
- Other meat and meat products
- Poultry and sea foods mainly fish
- Dried peas
- Beans and whole pulses
- Lentils (masoor)
- Mushrooms
- Spinach
- Cashew nuts and peanuts
- Alcohol
- Sweet bread and cheese
|
|
|
|